The word hysterectomy is derived from the ancient Greek terms for “womb” (hystéra) and “excision” or surgical removal (ektomé) — which pretty succinctly describes the process.
This surgery to remove the uterus (and, depending on your particular situation, the ovaries and Fallopian tubes may also be removed) means you will no longer have periods and can’t get pregnant. Below, find out more about the types of hysterectomies, how they’re done, and what to expect afterward.
Hysterectomy by the numbers
According to an American College of Obstetricians and Gynecologists (ACOG) report from 2017, hysterectomy is one of the most frequently performed surgical procedures in the United States. In fact, from 2000 to 2004, there were approximately 600,000 done each year.
The most common reasons women have hysterectomies are for symptomatic uterine fibroids (40.7%), endometriosis (17.7%), and prolapse (14.5%), per ACOG, and abdominal hysterectomy is performed in 66% of cases, vaginal hysterectomy in 22% of cases, and laparoscopic hysterectomy in 12% of cases.
Why would you need a hysterectomy?
The most common reasons women have this surgery include:
Uterine fibroids. Uterine fibroids are noncancerous growths in the wall of the uterus. In some women they cause pain or heavy bleeding.
Heavy or unusual vaginal bleeding. Changes in hormone levels, infection, cancer, or fibroids can cause heavy, prolonged bleeding.
Uterine prolapse. This is when the uterus slips from its usual place down into the vagina. This is more common in women who had several vaginal births, but it can also happen after menopause or because of obesity. Prolapse can lead to urinary and bowel problems and pelvic pressure.
Endometriosis. Endometriosis happens when the tissue that normally lines the uterus grows outside of the uterus on the ovaries where it doesn’t belong. This can cause severe pain and bleeding between periods.
Adenomyosis. In this condition, the tissue that lines the uterus grows inside the walls of the uterus where it doesn’t belong. The uterine walls thicken and cause severe pain and heavy bleeding.
Cancer (or precancer) of the uterus, ovary, cervix, or endometrium (the lining of the uterus). Hysterectomy may be the best option if you have cancer in one of these areas. Other treatment options may include chemotherapy and radiation. Your doctor will talk with you about the type of cancer you have and how advanced it is.
What are the different types of hysterectomies?
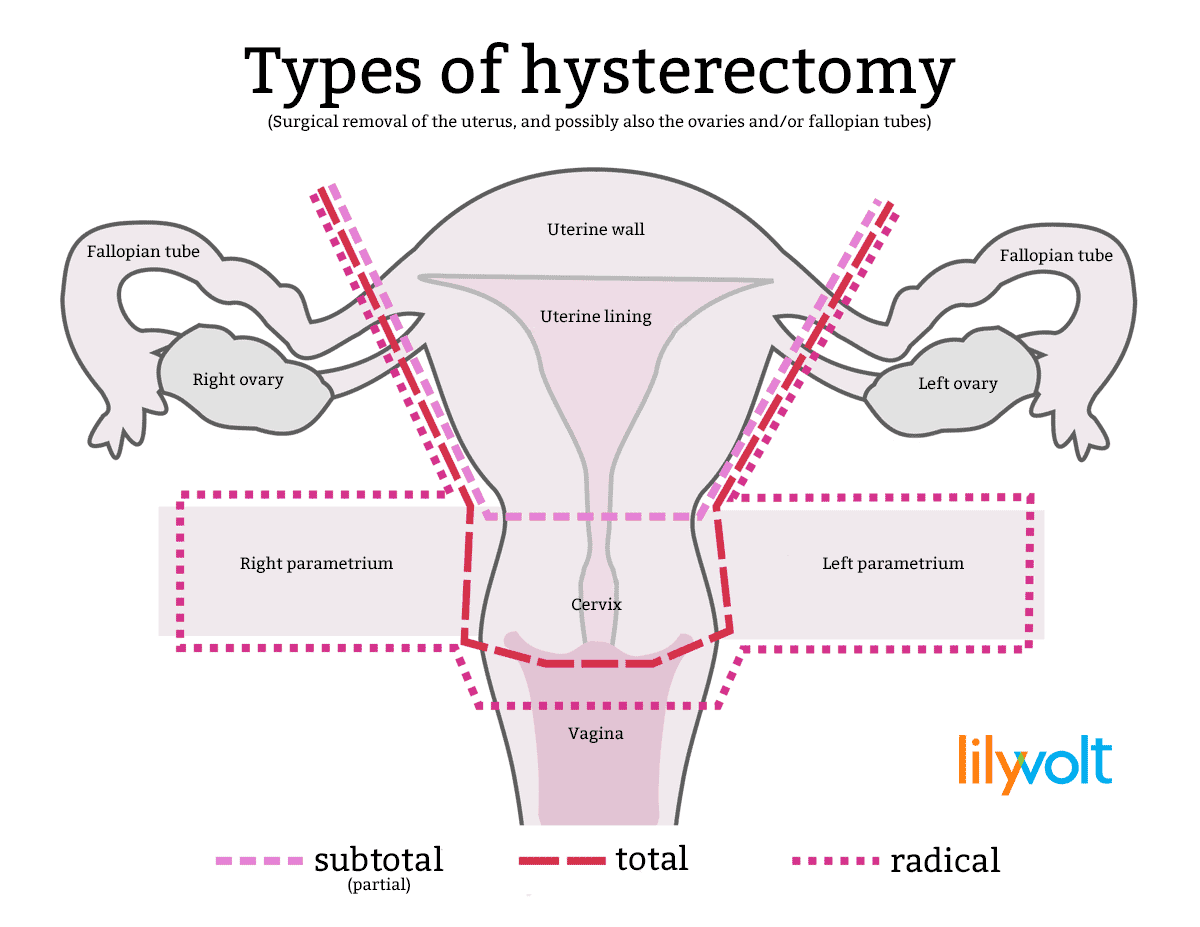
A total hysterectomy removes all of the uterus, including the cervix. The ovaries and the fallopian tubes may or may not be removed. This is the most common type of hysterectomy.
A partial, also called subtotal or supracervical, hysterectomy removes just the upper part of the uterus. The cervix is left in place. The ovaries may or may not be removed.
A radical hysterectomy removes all of the uterus, cervix, the tissue on both sides of the cervix, and the upper part of the vagina. A radical hysterectomy is most often used to treat certain types of cancer, such as cervical cancer. The fallopian tubes and the ovaries may or may not be removed.
Will the doctor remove your ovaries during the hysterectomy?
Whether your ovaries are removed during the hysterectomy may depend on the reason for your operation.
Ovaries may be removed during a hysterectomy to lower the risk for ovarian cancer. However, women who have not yet gone through menopause also lose the protection of estrogen, which helps protect women from conditions such as heart disease and osteoporosis.
Recent studies suggest that removing only the fallopian tubes — but keeping the ovaries — may help lower the risk for the most common type of ovarian cancer, which is believed to start in the fallopian tubes.
If both ovaries are removed, you will have symptoms of menopause, and hormone replacement therapy (HRT) may be recommended. On the other hand, if you keep one or both ovaries, you may still get some of the premenstrual and menstrual symptoms you had before — such as mood swings, tender breasts and headaches.
The decision to keep or remove your ovaries is one you can make after understanding the risks and benefits. Talk to your doctor well before your surgery to make sure you understand your options, and know what to expect afterward.
How is a hysterectomy performed?
A hysterectomy can be done in several different ways. It will depend on your health history and the reason for your surgery. Talk to your doctor about the different options:
Abdominal hysterectomy. Your doctor makes a cut, usually in your lower abdomen.
Vaginal hysterectomy. This is done through a small cut in the vagina.
Laparoscopic hysterectomy. A laparoscope is an instrument with a thin, lighted tube and a small camera that allows your doctor to see your pelvic organs. Laparoscopic surgery is when the doctor makes very small cuts to put the laparoscope and surgical tools inside of you. During a laparoscopic hysterectomy, the uterus is removed through the small cuts made in either your abdomen or your vagina.
Robotic surgery. Your doctor guides a robotic arm to do the surgery through small cuts in your lower abdomen, like a laparoscopic hysterectomy.
How long does it take to recover from a hysterectomy?
Recovering from a hysterectomy takes time. Most women stay in the hospital one to two days after surgery. Some doctors may send you home the same day of your surgery. Some women stay in the hospital longer, often when the hysterectomy is done because of cancer.
Your doctor will likely have you get up and move around as soon as possible after your hysterectomy. This includes going to the bathroom on your own. However, you may have to pee through a thin tube called a catheter for one or two days after your surgery.
The time it takes for you to return to normal activities depends on the type of surgery:
Abdominal surgery can take from four to six weeks to recover.
Vaginal, laparoscopic, or robotic surgery can take from three to four weeks to recover.
You should get plenty of rest and not lift heavy objects for four to six weeks after surgery. At that time, you should be able to take tub baths and resume sexual intercourse. How long it takes for you to recover will depend on your surgery and your health before the surgery. Talk to your doctor.
What changes can you expect after a hysterectomy?
Hysterectomy is a major surgery, so recovery can take a few weeks. But for most women, the biggest change is a better quality of life. You should have relief from the symptoms that made the surgery necessary.
Other changes that you may experience after a hysterectomy include:
Menopause. You will no longer have periods. If your ovaries are removed during the hysterectomy, you may have other menopause symptoms.
Change in sexual feelings. Some women have vaginal dryness or less interest in sex after a hysterectomy, especially if the ovaries are removed.
Increased risk for other health problems. If both ovaries are removed, this may put you at higher risk for certain conditions such as: bone loss, heart disease, and urinary incontinence (leaking of urine). Talk to your doctor about how to prevent these problems.
Sense of loss. Some women may feel grief or depression over the loss of fertility or the change in their bodies. Talk to your doctor if you have symptoms of depression, including feelings of sadness, a loss of interest in food or things you once enjoyed, or less energy, that last longer than a few weeks after your surgery.
Will the hysterectomy cause you to enter menopause?
All women who have a hysterectomy will stop getting their period. Whether you will have other symptoms of menopause after a hysterectomy depends on whether your doctor removes your ovaries (an oophorectomy) during the surgery.
If you keep your ovaries during the hysterectomy, you should not have other menopausal symptoms right away, but you may have symptoms a few years younger than the average age for menopause (51 years).
Because your uterus is removed, you no longer have periods… but your ovaries might still make hormones, so you may not have other (non-blood related) signs of menopause. You could have hot flashes, a symptom of menopause, because the surgery may have blocked blood flow to the ovaries, which can prevent the ovaries from releasing estrogen.
If both ovaries are removed during the hysterectomy, you will no longer have periods, and you may have other menopausal symptoms right away. Because your hormone levels drop quickly without ovaries, your symptoms may be stronger than with natural menopause. Ask your doctor about ways to manage your symptoms.
If one ovary is removed, your body may take several months to adjust, but the remaining ovary will typically take over for its missing counterpart. As stated in the Encyclopedia of Family Health, “What usually happens when one ovary is removed is that the other one grows slightly larger and takes over the work of both ovaries.”
Will your sex life change after a hysterectomy?
It might. If you had a good sex life before your hysterectomy, you should be able to return to it without any problems after recovery. Many women report a better sex life after a hysterectomy because of relief from pain or heavy vaginal bleeding.
If your hysterectomy causes you to have symptoms of menopause, you may experience vaginal dryness or a lack of interest in sex. Using a water-based lubricant can help with dryness. Talk to your partner and try to allow more time to get aroused during sex. Talk with your healthcare provider for additional advice.
Do you still need to have Pap tests?
Maybe. You will still need regular Pap tests (aka Pap smear) to screen for cervical cancer if you did not have your cervix removed, or if you had a hysterectomy because of cancer or precancer. Ask your doctor what is best for you and how often you should have this test done.
What are some alternatives?
Hysterectomy is major surgery. Sometimes a hysterectomy may be medically necessary, such as with prolonged heavy bleeding or certain types of cancer. But sometimes you can try another thing first, such as:
Watchful waiting. You and your doctor may wish to wait if you have uterine fibroids, which tend to shrink after menopause.
Exercises. For uterine prolapse, you can try Kegel exercises (squeezing the pelvic floor muscles). Kegel exercises help restore tone to the muscles holding the uterus in place.
Medicine. Your doctor may give you medicine to help with endometriosis. Over-the-counter pain medicines taken during your period also may help with pain and bleeding. Hormonal birth control, such as the pill, shot, or vaginal ring, or a hormonal intrauterine device (IUD) may help with irregular or heavy vaginal bleeding or periods that last longer than usual.
Vaginal pessary (for uterine prolapse). A pessary is a rubber or plastic donut-shaped object, similar to a diaphragm used for birth control. The pessary is inserted into the vagina to hold the uterus in place. Uterine prolapse happens when the uterus drops or “falls out” because it loses support after childbirth or pelvic surgery.
Surgery. You and your doctor may choose to try a surgery that involves smaller or fewer cuts than a hysterectomy, helping you heal faster with less scarring.
Treatments to shrink fibroids without surgery. These treatments include uterine artery embolization (UAE) and magnetic resonance (MR)-guided focused ultrasound (MR[f]US).
UAE puts tiny plastic or gel particles into the vessels supplying blood to the fibroid. Once the blood supply is blocked, the fibroid shrinks and dies. MR(f)US sends ultrasound waves to the fibroids that heat and shrink the fibroids. After UAE or MR(f)US, you will not be able to get pregnant.